- Fentanyl is a synthetic opioid (pain medication) commonly used as a drug of abuse
- It comes as a powder, tablet or liquid
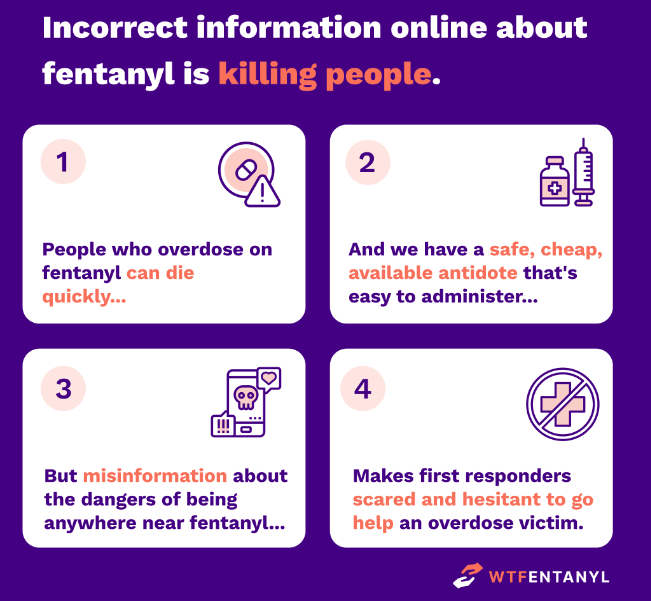
- It is not absorb through touch
- It is not absorbed by breathing in close proximity to the powdered drug
- No confirmed case of passive (not ingested/injected) fentanyl exposure has ever been documented
- Fentanyl overdose is treated with Narcan(naloxone) given by nasal spray or injection
- Narcan (naloxone) should be administered to anyone who is unresponsive or has slow or shallow breathing
What is Fentanyl?
Fentanyl is a medication used to rapidly treat severe pain by injection through an IV (intravenous) by EMS and hospital providers. It is a synthetic opioid similar to tramadol and methadone. Unlike naturally occurring opiates such as morphine that was originally distilled from the opium plant, synthetic opioids are produced in labs to alter how the drug affects the body. In the case of fentanyl it works faster and is more potent (lower dose causes same effect) than morphine. This makes it an ideal drug for the management of severe pain by medical providers where fast and powerful pain control is needed to diagnose and treat injuries. Medicinal fentanyl is produced in a liquid form used in IV medication, as a muscular injection or in a specialized skin patch. For children it also comes in an intranasal form. It has also become increasingly popular as a drug of abuse due to its fast and long lasting high in very small doses.
| Opiates | Synthetic opioids |
|---|---|
| Morphine | Fentanyl |
| Heroin | Methadone |
| Codeine | Tramadol |
Opiates refer to natural opioids such as heroin, morphine and codeine.
Opioids refer to all natural, semisynthetic, and synthetic opioids including fentanyl.
What does Fentanyl do?
Fentanyl acts primarily on the opioid receptors in the brain decreasing the sensation of pain and stimulating the release of reward hormones causing a sense of euphoria. As the dose increases it also effects other receptors leading to the many side effects common to all opioid medications. These include constipation, nausea, vomiting, confusion, sedation and respiratory depression. All opioids have a similar chemical structure and effects on the body as the naturally occurring opiates that have been distilled from opium plants for thousands of years. Pharmaceutical companies have since created dozens of drugs within the opioid class to treat pain. Some common forms include the pill oxycodone which is absorbed slowly and more consistently over several hours when compared to the intravenous drugs like fentanyl which act in minutes.
Fentanyl is used by medical providers because of its rapid ability to decrease pain and when given in higher doses can be used to sedate a person for emergency procedures like intubation (placing a breathing tube). The most dangerous side effect, and the cause of an overdose, is the effect opioids have on breathing. In high doses opiates decrease, or stop, the body from “remembering” to breath which can lead to cardiac arrest and death. The other side effects such as nausea, confusion, sedation and constipation are often experienced by post surgical patients in the hospital. The severe constipation can even become life threatening in chronic users when it causes obstruction and rupture of their intestines leading to a surgical emergency.
Another effect of repeat opiate use is the development of a tolerance. This means that each repeat dose has to be higher than the previous to have the same effect. This is one of the reasons that pain control in opiate abusers is so difficult to manage because chronic users may need significantly lager doses than average to achieve similar pain control. Repeat use has also been linked to hyperalgesia which means that the person has an increased sense of pain. This is why some people on high doses of opiates may feel significantly more pain with things like IV insertion than someone else. Unfortunately, while people become tolerant to the pain reduction effects of the fentanyl they are still susceptible to the side effects of respiratory depression and constipation.
How strong is fentanyl?
Fentanyl is often described as being 50-100 times stronger than morphine and while this is true it is also important to know that the doses of fentanyl given in hospitals is significantly less than that of morphine and they are measured in different units. Medicinal fentanyl is typically measured in micrograms abbreviated mcg or μg with a typical adult dose being 25-50mcg by IV. Morphine is typically dosed in milligrams or mg with a typical dose being 4mg. A microgram is 0.001 milligrams or put another way, 1 microgram is one thousand times smaller than 1 milligram. So a 25mcg dose of fentanyl is 0.025mg around 160 times smaller than the morphine dose. All this means that when a person is given fentanyl or morphine in a hospital they are getting around the same effect because the doses have been adjusted to account for fentanyl’s increased potency.
Now, in the illicit drug trade fentanyl’s significant potency, and increased euphoria effect, makes it an ideal drug of trade. Not only can it be produced in a lab with chemicals ordered online, no large fields of crops needed, but it is more profitable by weight than other drugs. Pencil tip size doses of fentanyl can get a customer high, or overdose, so smaller amounts can be trafficked for higher profit.

Is fentanyl in the air?
No, due to fentanyl’s very low vapor pressure (4.6 x 10-6 Pa) it does not become a gas at room temperature or aerosolize enough to cause affects on people. Their are aerosolized forms of fentanyl that are given as medication but this requires specialized devices that use heat and compressed gasses to aerosolize the fentanyl directly into a persons nose or mouth. This is not a very effective way of administering the drug in high quantities and is why it is rarely used in hospitals. In factories that produce fentanyl they have calculated that an exposure to the highest possible air levels of fentanyl would require 200 minutes of exposure before causing effects. An interesting side note is the Russian Moscow Theatre hostage event where the Russian government released a gas containing synthetic opiates similar to fentanyl in an attempt to subdue the hostage takers. Unfortunately this resulted in the death of 125 people. However, it is important to note that additional substances, such as a gas used in anesthesia, were also a part of the mixture. No reported case of aerosolized fentanyl exposure has ever been reported in the United States.
Intranasal, the way Narcan is usually given, is another way to give fentanyl that is effective only in smaller doses due to poor absorption. This is why it is usually only used in children who require smaller doses. It also takes around 5 – 15 minutes for it to be absorbed through the mucous membranes of the nose. However, snorting a line of powdered fentanyl can result in a lethal doses but is very different from walking into a room or opening a car trunk with powdered fentanyl in it. The position statement on fentanyl by the American College of Medical Toxicology (ACMT) and American Academy of Clinical Toxicology (AACT) recommends that in rare instances where significant amounts of powdered fentanyl is in the air a N95 mask and eye protection should provide sufficient protection. These are the same recommendations as for handling a patient with COVID19 or the flu.

How is fentanyl absorbed?
Medical fentanyl is administered primarily by the intravenous route (IV) because this is the fastest way for a person to feel the effects of a medication working. Fentanyl can cause effects in less than 60 seconds of injection. This rapid effect can also cause a sense of euphoria and make someone “high” if a large enough dose is rapidly injected. The effects of IV fentanyl only last around 30-60 minutes when given in normal doses and is why illicit fentanyl is often mixed with other drugs to create a longer lasting high. Since fentanyl works almost immediately after injection it is an ideal pain medication for EMS providers to give patients until arrival to the emergency department. Fentanyl can also be given as an intramuscular injection when an IV is unable to be placed and takes around 8 minutes to have effects lasting 1-2 hours. Fentanyl can also be given as a skin patch that takes hours to take effect and can last for days. Its important to remember that significant research and special formulation went into the development of fentanyl patches because it is very difficult to get drugs absorbed through the skin. Even with specially formulated patch’s it takes hours for enough drug to be absorbed. This is one reason why some medication patches are chewed by people looking to get high because the drug can be absorbed faster through the mucous membranes of the mouth than the skin. While it is possible to overdose from wearing a fentanyl patch, simply touching one will not result in long enough contact for any amount of the drug to be absorbed. Overdoses from fentanyl patches can occur in young children who chew on the patches or in adults who simultaneously take other drugs or alcohol while wearing the patch. Once removed from the skin fentanyl that was in the outer layer of the skin continues to be absorbed over the next 12 hours so overdose can still occur after the patch has been removed. Other forms such as nasal sprays, nebulizers and sublingual strips are far less commonly used because they work slower and are more difficult to get maximum effect. Intranasal is more commonly used for children because the larger doses required by adults can not be well absorbed through the nose in a controlled fashion.
| Intravenous Fentanyl | Intramuscular Fentanyl | Intranasal Fentanyl | |
|---|---|---|---|
| Dose | 25-50 mcg | 25-50 mcg | 1.5mcg/kg (kids) |
| Time to affect | seconds | 8 minutes | 10 minutes |
| Duration of effect | 30-60 minutes | 1-2 hours | 1 hour |
Their are numerous ways that fentanyl can be used as a drug of abuse other than intravenous injection. Skin popping is the injection of fentanyl under the skin resulting in a slower absorption and not requiring a vein. It can also be injected deeper directly into a muscle such as the deltoid for similar effect. Fentanyl powders can be snorted leading to variable absorption and time to cause effect because some of the drug is absorbed faster through the mucous membranes of the nose and some of the drug is swallowed having a longer effect. Fentanyl pills are also being produced to imitate other common pain medication pills and have delayed effects due to the prolonged absorption in the intestines. They are often pressed into pills that look identical to other prescription opioid pills like oxycodone but unlike oxycodone act faster and are stronger. The One Pill Can Kill Campaign was created to inform the public about these fake pills. Smoking fentanyl involves heating the powdered drug, usually on aluminum foil, and inhaling the vapors. This can lead to rapid absorption similar to snorting the drug but can also lead to dangerous airway burns. One “benefit” of smoking is the decreased chance of spreading infections such as HIV between users since no needles are used. However, smoking can cause significant damage the airways and lungs and it is very difficult to predict the amount of drug a person will absorb.
An important constant in all of the ways that fentanyl is abused is none of them include touching or just being near the drug. In order to absorb significantly high enough doses to produce symptoms or overdose the drug must enter the body either invasively by a needle or by snorting the powder or inhaling a heated mixture. The most likely dangerous exposure a first responder will encounter is an accidental needle stick. This is an unfortunately common experience for first responders and medical professionals.
The greater risk from needle sticks is in the transmission of infectious diseases like HIV or Hepatitis C which can be transmitted by contact with a bloody needle. However, receiving a high enough dose of fentanyl, or any opiate, by an accidental needle stick is very unlikely. If you or anyone else have their skin punctured by a dirty needle you should immediately rinse the wound with potable water and go to the emergency department for evaluation. Early treatment can prevent infection but becomes less effective the longer you wait. The same procedure should be followed any time your skin is broken by an object that has come in contact with the bodily fluids of another person. As well as anytime you get blood from another person in your mucous membranes (eyes, mouth, nose). While transmission of infectious disease is unlikely in these scenarios early preventative treatment can decrease your risk even further.
What is Fentanyl withdrawal?
All opiates when taken over time can lead to dependence, this means a person feels negative effects when they are not taking the drug. Withdrawal is a process where the body has to get used to the lack of a drug causing various symptoms. The severe diarrhea, pain, nausea, vomiting, sweating, and insomnia from withdrawal can last up to weeks depending on how much of the drug the person had been using and for how long. Symptoms of withdrawal can be managed by prescription medications such as methadone under the direction of a medical provider. Unlike withdrawal from alcohol withdrawal from opiates like fentanyl are very rarely fatal but do cause significant distress often causing people to return to opiate abuse to reduce their symptoms. Even years after successfully stopping opiate use many people will continue to have cravings and will take medications such as suboxone on a daily basis to reduce symptoms of craving. The extreme difficulty some people have in quitting opiates is one reason why some patients will refuse opiate medications such as morphine or fentanyl despite severe injury or pain. It is also very common for people who have been addicted to substances to have periods of relapse and sobriety. Remember, as first responders we only see the people who are addicted or have relapsed, we do not get called to see the people who have successfully overcome addiction!
Additional Resources
- American College of Medical Toxicology Statement on Fentanyl Exposure and other resources: https://www.acmt.net/fentanyl-exposure-resources/
- WTFentanyl is a website dedicated to dispelling fentanyl exposure myths written by physician specialists: https://wtfentanyl.com/